An Australian man with heart failure has become the first person in the world to survive more than 100 days with an artificial titanium heart as he waited to receive a donor transplant.
The breakthrough raises hopes that fully mechanical hearts could one day replace the need for donor transplants.
Diseases of the heart and surrounding blood vessels are the leading cause of death globally, killing about 17.9 million people each year, according to the World Health Organization.
Here’s what to know about how the titanium heart works, and can it solve the global donor shortage?
What happened with the man with an artificial heart?
The man in his forties, who declined to be identified, became the first person to be discharged from hospital with a fully artificial heart implant.
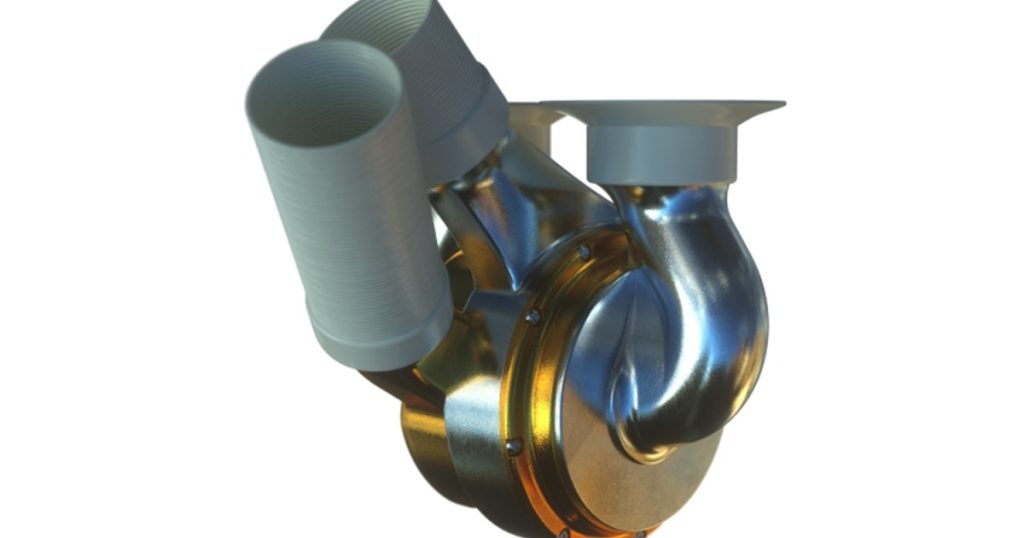
During a six-hour surgery in November 2024 at St Vincent’s Hospital in Sydney, the BiVACOR Total Artificial Heart (TAH) made of titanium was implanted into the patient, who was experiencing severe heart failure.
After spending a few weeks in intensive care, followed by observation in the hospital, the patient was discharged in early February.
He lived with the artificial heart for 105 days before receiving a donor heart transplant on March 6, and is currently recovering well, according to his doctors.

Has anyone else had a titanium heart transplant?
In July 2024, a 57-year-old man with end-stage heart failure received the BiVACOR TAH at Baylor St Luke’s Medical Center in Houston, Texas.
This was the first human implantation of the titanium heart, serving as a bridge to a real heart transplant. The device supported the patient for eight days in the hospital until a donor heart became available.
Between July and November 2024, four other men in their mid-forties to mid-sixties in the US also received the BiVACOR TAH. Each patient successfully transitioned to a donor heart transplant and was discharged from the hospital within a month. None of the US patients left the hospital with the device.
Could it solve a heart donor shortage?
The titanium heart could possibly help address the donor shortage by keeping patients alive while they wait for a real heart transplant. However, it is still uncertain whether it could ever serve as a permanent replacement for a human heart.
The procedures in the US, for example, were part of a five-person early feasibility study approved by the country’s Food and Drug Administration (FDA), with plans to expand the trial to 15 more patients in the coming months. The goal of such trials is to determine whether the titanium heart can safely keep patients alive while they wait for a transplant.
Finding a donor heart isn’t easy because there aren’t enough available, and matching a heart to a patient can take time. In the United Kingdom, for example, patients on the regular waiting list for a donor heart usually wait 18 to 24 months. Those in urgent or emergency cases get priority and may receive a heart sooner because their condition is more critical.
Heart failure affects at least 26 million people worldwide, including 6.2 million adults in the US. However, heart transplants remain rare, with fewer than 6,000 performed globally each year, reserved only for the most severe cases.
How does a titanium heart work?
The titanium artificial heart works very differently from a real heart. A natural heart beats by squeezing and relaxing to pump blood, but this artificial heart does not beat at all.
Instead, it has a spinning disc inside that moves the blood around the body. This disc floats in place using magnets, so it never touches anything, meaning there’s no friction and less chance of it wearing out over time.
To keep running, the artificial heart needs a small external controller, which is powered by batteries during the day and plugged into a power source at night. A thin cable runs under the skin to connect the heart to this controller.
Most artificial heart devices only replace one side of the heart, usually the left side. But the BiVACOR heart completely replaces the entire organ, making it an option for people whose whole heart is failing and who might not survive while waiting for a donor heart.
Why was titanium chosen for an artificial heart?
Titanium was chosen because it is strong, lightweight, and resistant to corrosion, making it ideal for long-term use in the body. Unlike other artificial hearts, which have multiple moving parts that can wear out, this one has only one spinning disc, reducing the risk of failure.
Before the development of the BiVACOR artificial heart, the SynCardia Total Artificial Heart was the most commonly used device for patients with severe heart failure.
Approved by the FDA in the early 2000s, the SynCardia heart is constructed primarily from polyurethane, a type of durable plastic. Over the past two decades, it has been temporarily implanted in more than 2,000 patients across 20 countries while they awaited donor heart transplants. However, the SynCardia device is relatively large and complex, with multiple moving parts that can wear out over time.
Scientists have also explored using animal organs to treat heart failure. In January 2022, surgeons at the University of Maryland Medical Center in the US performed the first transplant of a genetically modified pig heart into a human patient with severe heart disease.
Despite initial success, the patient developed complications and passed away approximately two months later.
How long could a titanium heart last?
Currently, no one knows the exact lifespan of the titanium heart in humans. In lab tests, the device has operated continuously for more than four years without signs of failure.
While the Australian man’s 100-day trial was the longest recorded use of the titanium heart in a human, the BiVACOR team has said further trials are needed to determine whether it could become a long-term replacement rather than just a temporary bridge to a transplant.
The development of the device began in 2001 when Daniel Timms, inspired by his father’s heart condition, started working on the concept during his PhD at Queensland University of Technology in Australia. Since then, it has undergone years of research, redesign, and testing in animals like calves and pigs.
What challenges come with an artificial heart?
One of the biggest challenges with organ transplants is immune rejection, where the body attacks the new organ as a foreign object.
Since the BiVACOR titanium heart does not contain any biological tissue, the risk of rejection is lower compared with donor hearts or pig heart transplants. However, trial protocols indicate patients still take blood-thinning medication to prevent clotting around the device.
Additionally, patients with the BiVACOR heart must stay connected to an external power source at all times.
While portable battery packs allow for some mobility, the process still requires lifestyle adjustments such as battery recharging, avoiding activities that could damage the external parts, and planning travel carefully to ensure access to power.